Vitamin D: an expert view

Dr Nicholas Shenker PhD FRCP, is a consultant rheumatologist at Addenbrooke’s Hospital in Cambridge and an expert in chronic pain syndromes. He is a member of the medical advisory board at Cambridge Nutraceuticals.
Here, Dr Shenker presents the scientific facts about vitamin D and shares his own perspective about the vital nutrient as an authority on bone and joint health.
- The facts
- Vitamin D deficiency

- When to take a vitamin D blood test
- Who should take vitamin D?
- Replacement therapy
- Supplements
- Who should take vitamin D?
- What are the risks of replacing vitamin D?
- Summary
The facts
Vitamin D is essential for musculoskeletal health. It allows calcium absorption from the bowel, enables mineralisation of newly formed bone, and plays an important role in muscle function. The parathyroid hormone counteracts vitamin D in the body by removing calcium from bone and excreting it through the kidney. Vitamin D and Parathyroid hormone therefore counterbalance each other to keep the level of calcium in the blood and bone at a stable level.
Vitamin D is a fat-soluble vitamin and needs sunlight to convert it to the more active form in the body. The liver and kidney have key functions in modifying the vitamin D to convert it into its final form. If the liver or kidneys are not working well, vitamin D levels are affected. Supplying the body of someone with poorly functioning kidneys or liver with the right form of vitamin D is more complicated – this is achieved using with calcitriol (1, 25 –vitamin D).
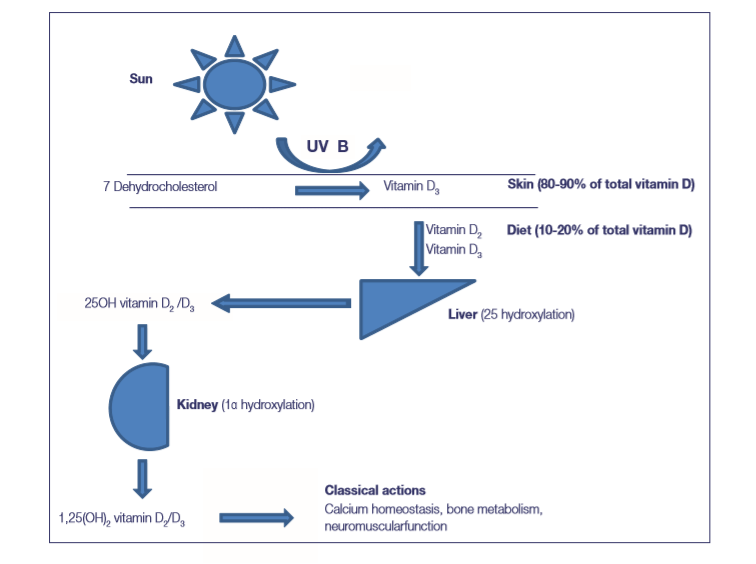
Figure 1: How vitamin D is made in the body
Sun exposure is crucial for the formation of vitamin D. In the summer, you should spend 10 minutes outside between 10am and 3pm on a clear day, three times a week, to generate enough. Spending much longer will not convert more vitamin D. Getting sunlight 'little and often' is the best strategy for creating vitamin D, as this helps you to avoid sun exposure, which is a risk factor for skin cancer.
Vitamin D is found in fatty fish, fish oils, liver and eggs. In the UK, margarine, powdered milks and cereals are often fortified with vitamin D.
Vitamin D deficiency
|
Vitamin D level |
Deficiency (as measured in a blood test) |
|
< 20 nmol/L |
Deficient |
|
20-50 nmol/L |
Insufficient |
|
50-75 nmol/L |
Acceptable |
|
75-100 nmol/L |
Probably the optimum |
|
> 200 nmol/L |
Too much |
If you are low in vitamin D, it can cause a condition known as osteomalacia in adults and rickets in children. Too little calcium in your bones will cause them to become ‘soft’ and more likely to fracture. The Department of Health suggests that this softening of the bone can occur at levels of serum 25 hydroxyvitamin D (25OHD) concentration of less than 20nmol/L. The optimal level of vitamin D is more than 50nmol/L and possibly between 75-100nmol/L.
Less severe vitamin D deficiency, sometimes termed vitamin D insufficiency, may still lead to secondary hyperparathyroidism (an overreaction in the parathyroid gland when vitamin D levels are low); bone mineral loss; muscle weakness; and falls and fragility fractures in older people.
Figure 2: Scheme of who to test and potentially treat with vitamin D replacement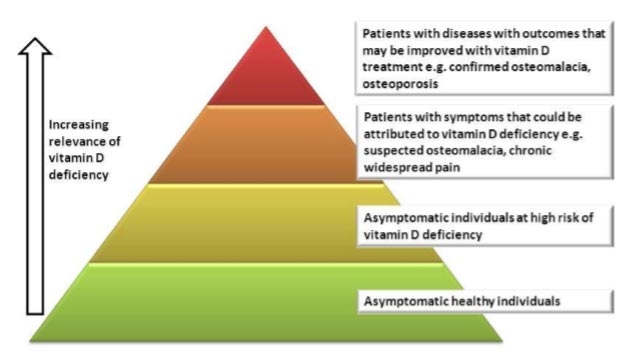
When to take a vitamin D blood test
Most people do not need to check their vitamin D levels.
People with recurrent fractures, particularly low impact (fragility) fractures should have their vitamin D checked, as should those with osteoporosis, osteomalacia or stress fractures. Those with generalised fatigue, weakness or chronic widespread pain should also consider having their vitamin D checked.
There are also groups that are at a high risk of deficiency, whose members could benefit from a check. These at-risk groups include:
- Pregnant or breastfeeding women
- People with darker skin (African, South Asian or Afro-Caribbean)
- People who cover up in the sunshine (for example, for cultural reasons)
- People who are housebound
Who should take vitamin D?
People can take vitamin D either as a supplement to their diet or to replace low levels of vitamin D.
Replacement therapy with high doses of vitamin D (see below) should be given to those who are deficient in vitamin D (<20nmol/L).
People who are insufficient in vitamin D (20-50nmol/L) should also commence a replacement regimen if they:
- have had a fragility fracture (the result of a fall from a standing position onto carpeted/soft ground).
- Have a documented case of osteoporosis (following a bone density scan, e.g. DEXA).
- Have a high fracture risk (as assessed by known risk factors such as rheumatoid arthritis, inflammatory bowel disease, coeliac disease, early menopause, family history, heavy alcohol intake, hyperparathyroidism, hyper- or hypothyroidism).
- Are about to start treatment with antiresorptive medication for bone disease (e.g. a bisphosphonate).
- Experience symptoms suggestive of vitamin D deficiency (weakness, fatigue, widespread pain).
- Are at increased risk of developing vitamin D deficiency in the future because of reduced exposure to sunlight, religious/cultural dress code, or dark skin.
- Are taking medication with antiepileptic drugs or oral glucocorticoids (steroids).
Replacement therapy
Replacement regimens for the treatment of deficiency suggest doses of vitamin D up to a total of approximately 300,000 IU, given either as weekly or daily split doses. The exact regimen will depend on the local availability of vitamin D preparations, but examples include:
- 50,000 IU capsules, one given weekly for six weeks (300,000 IU)
- 20,000 IU capsules, two given weekly for seven weeks (280,000 IU)
- 800 IU capsules, five a day given for 10 weeks (280,000 IU)
The following should be borne in mind:
- Supplements should be taken with food to aid absorption.
- Tablets that include calcium in addition to vitamin D should not be used as sources of vitamin D for the above regimens, given the resulting high dose of calcium.
Once the replacement regimen has finished, a maintenance regimen may be considered one month later. This regimen recommends doses equivalent to 800 to 2,000 IU daily (occasionally up to 4,000 IU daily), given either daily or intermittently at a higher equivalent dose.
Supplements
A minimum of 400 IU (10μg) daily is recommended for:
- All pregnant or breastfeeding women
- Anyone older than 65 who does not get much sun exposure
- All people with dark skin (African, South Asian, Afro-Caribbean)
- All people who cover up in the sunshine (e.g. for cultural reasons) or are housebound
There is good evidence that taking 25μg daily (1,000 IU) is safe, and it has been shown to increase life expectancy in an elderly population.
Supplementing someone’s diet with 1,000 IU (25μg) of vitamin D will raise their vitamin D between 25-30nmol/L. This will slowly rise to reach a steady state in three to six months.
Calcium and vitamin D
Calcium calculators can help you to establish how much calcium you might be consuming every day.
If patients with osteoporosis are found to not be reliably or regularly consuming at least 700mg calcium per day, titrated supplementation with either calcium-only supplements or calcium and vitamin D combined supplements is recommended.
There is some concern that too much calcium can cause heart attacks and strokes due to a ‘hardening’ of the arteries. This is an area of active research.
What are the risks of replacing vitamin D?
Replacing vitamin D can lead to a high calcium level due to unmasking of hyperparathyroidism. People might feel unwell. They might be very thirsty, feel low in their mood or have abdominal pains. A blood test to look for a raised calcium level can screen for hyperparathyroidism - this can be organised through a GP.
The European Food Safety Authority (EFSA) has reviewed the evidence and concluded that an upper limit of 4,000 IU (100µg) of vitamin D per day is safe for adults and children over 11 years of age.
Very rare conditions, including tuberculosis and sarcoidosis can be associated with high levels of calcium after vitamin D is replaced. Special advice is usually sought for people with these conditions.
Finally, high levels of vitamin D can cause a build-up of calcium in the kidney, resulting in kidney stones.
Summary
Vitamin D is essential to musculoskeletal health because of its role in mineralizing bone.
It is important to follow government guidelines on vitamin D intake. By taking NHS advice you will ensure that you are generating enough in your skin, getting enough from your diet and taking a supplement of the recommended strength to prevent deficiency.
References
National Osteoporosis Society. Vitamin D and bone health. A practical Clinical Guideline for patient management. April 2016
